Earlier this year, the Centers for Medicare & Medicaid Services (CMS) released the 2024 National IMPACT Assessment Report—an analysis evaluating the performance of various healthcare quality measures nationwide. In care management, you know these updates can significantly alter your day-to-day operations—especially in areas like care coordination, post-acute discharge planning, and compliance with federal value-based care standards.
What do these recent insights mean for your healthcare organization? And how can Aidin’s referral management software help support your efforts to simplify and enhance your compliance operations—all while improving patient outcomes and satisfaction?
What is the CMS 2024 National IMPACT Assessment Report?
CMS’s 2024 National IMPACT Assessment reviews progress providers have made over the past three years in implementing data standardization and quality reporting requirements mandated by the IMPACT Act of 2014. This legislation was passed to improve care coordination across post-acute care settings such as home health agencies (HHAs), skilled nursing facilities (SNFs), inpatient rehabilitation facilities (IRFs), and long-term care hospitals (LTCHs). Notably, this law requires these organizations to collect and share standardized data on patient outcomes, resource utilization, and quality of care. Specifically, the original Act’s mandates relate to:
- Data standardization: The Act requires post-acute care providers to collect and report standardized data on patient outcomes, quality of care, and resource use. The purpose of this rule is to ensure uniformity and comparability across different settings.
- Care coordination: By focusing on data interoperability, the Act aims to enhance care transitions between healthcare providers, ultimately improving care continuity and reducing hospital readmissions.
- Patient-centered decision-making: Providers must share quality and resource use data with patients during discharge planning to help them make informed choices about post-acute care services.
Quality reporting: The IMPACT Act mandates that post-acute care providers report data that measures quality and efficiency, aligning with broader CMS initiatives to improve transparency and accountability in healthcare.
What are some of the 2024 report’s key highlights?
While the 2024 assessment doesn’t introduce new policies, it provides valuable insights into how well providers have met the goals outlined in the 2014 IMPACT Act. Here are some of the key findings:
- Increased use of standardized data: The assessment shows significant progress in collecting and reporting standardized patient data by providers—crucial processes for comparing quality of care across different post-acute care settings.
- Gaps in compliance and reporting: Some providers still struggle with data reporting consistency—especially for resource use metrics and patient-reported outcomes that are key to meeting the goals of the IMPACT Act.
- Safety declines: Based on 2016–2019 trends, patient safety measures declined by 38% in 2020 and 47% in 2021. CMS attributes this downward trend to disruptions likely caused by the COVID-19 pandemic.
- Impact on patient outcomes: Providers implementing the IMPACT Act’s guidelines fully saw improvements in care transitions and patient satisfaction. However, the assessment also highlights that more work is needed to streamline care coordination—particularly for hospital discharge to post-acute care—to meet the Act’s expectations.
- Transitions of care challenges: Providers face issues when ensuring seamless care transitions between acute and post-acute care providers—particularly when sharing up-to-date, actionable steps with patients and families at the point of discharge.
What do these outcomes mean for care management today and in the future?
This 2024 CMS assessment serves as a performance report on how well the industry has adapted to the 2014 IMPACT Act. While many health systems and providers have made strides in meeting reporting and care coordination requirements, they must face a few distinct challenges to satisfy goals established by the original legislation. This year’s report underscores the need for continued focus on:
- Data-sharing: Providers must remain diligent in collecting and sharing standardized quality and resource-use data. This information not only impacts compliance but it also supports better care coordination across stakeholders.
- Patient-centered discharge planning: The 2014 IMPACT Act requires that hospitals help patients select post-acute care providers using real-time quality data that aligns with treatment plans and goals. Healthcare organizations must deliver accurate, up-to-date information to help patients make informed choices.
- Efficiency during transitions of care: Effective care transitions between hospitals and post-acute care settings are crucial to improving outcomes, reducing length of stay, and mitigating readmissions. Successful transitions require integrating technology that supports real-time communication and decision-making among providers, patients, and families.
How do CMS’s latest Home Health Payment Rule updates relate to these findings?
CMS has released the final Home Health Payment Rule for 2024, introducing several key changes to Medicare payments and related policies for home health agencies. As these organizations deliver post-acute care, they will need to reach significant improvements to both uphold IMPACT standards and satisfy these updates—especially where priorities overlap, such as improving patient outcomes and standardizing data.
Some highlights from this rollout include:
- Payment adjustments: The rule includes a modest 0.8% net increase in Medicare payments for home health agencies in 2024, reflecting a balance between inflationary updates and behavioral adjustments.
- Behavioral adjustment phasing: CMS continues phasing in behavioral rate adjustments, which were initially introduced under the Patient-Driven Groupings Model (PDGM) to address changes in provider behavior. This measure ensures that payments remain aligned with actual care needs rather than inflated projections.
- Expansion of value-based purchasing: The Home Health Value-Based Purchasing (HHVBP) model has been extended, incentivizing agencies to improve care quality. Agencies are evaluated on metrics such as hospital readmissions and patient satisfaction, and their payments are adjusted based on performance.
- Equity and data transparency: CMS has included provisions to enhance care delivery equity and standardize data reporting. This move aims to address disparities and improve care quality and outcomes transparency.
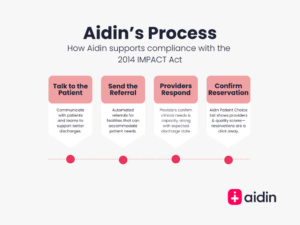
How can Aidin support your compliance needs, including the 2024 IMPACT Assessment updates?
- Optimizing patient choice: Aidin helps significantly improve patients’ selection of their post-acute care providers. In traditional discharge planning models, only 16% of patients choose the provider with the highest quality ratings. However, with Aidin’s updated discharge planning platform and process, 85% of patients select top-rated providers, significantly improving their outcomes. This shift is transforming the process for all involved—care management teams, post-acute providers, and most importantly, patients and their families.
- Reducing length of stay: Aidin’s platform enables more efficient care management workflows, and tools have consistently demonstrated a reduction in LOS. By helping case managers coordinate care and transition patients smoothly to appropriate post-acute care settings, Aidin has reduced the average LOS for post-acute discharges by almost a full day.
- Ensuring compliance and transparency: Aidin’s system is built with compliance in mind, ensuring that hospitals can meet the latest requirements for discharge planning. Our tools automatically collect and share the necessary quality data with patients and their families, verifying that they have all the information needed to make informed choices that will yield the best outcomes from hospital discharge to post-acute care.
- Ongoing compliance support: Aidin works closely with your compliance teams to ensure that our tools, workflows, and reporting are always aligned with CMS regulations. We regularly update our platform to reflect any changes in policy so that you can focus on patient care without worrying about compliance.
- Simplified hospital workflows: As a platform designed to streamline multiple care management workflows in one place, Aidin enables health systems to optimize shared workflows with payers and post-acute providers, ensures updated processes are fully interoperable, and establishes incentives (badges) that reward successful partnerships. This comprehensive approach leads to better productivity, less operational friction, and more win-wins for care teams and patients.
Download a white paper: Learn more about streamlining care management workflows and reducing costs.
What are some next steps for care management leaders?
Staying ahead of the curve is critical. If you’re leading care management at a health system, some actionable steps include:
- Re-review the full 2024 National IMPACT Assessment Report to comprehensively understand how your facility aligns with industry-wide performance trends and regulatory expectations. By examining the findings, you can identify potential gaps in compliance, areas for improvement, and opportunities to enhance patient care.
- Take note of valuable benchmarks that can help you assess your facility’s performance relative to national standards, ensuring you stay compliant with CMS requirements and continuously improve care delivery. Ensuring you have clear visibility into the data across all areas of care management and throughout the referral management process with a platform like Aidin can help you know exactly where issues are occurring.
- If necessary, refine your discharge planning processes to align with CMS requirements, particularly those pertaining to sharing quality and resource use data. CMS mandates that hospitals provide patients with detailed information on post-acute care providers upon discharge. This empowers patients to make informed decisions about their care transitions and ensures compliance with regulations under the IMPACT Act. There are ways to leverage technology, such as Aidin, to streamline updates.
- Consider partnering with a trusted referral management software like Aidin to streamline transitions of care, improve patient outcomes, and ensure compliance with evolving federal regulations. Aidin’s comprehensive care coordination platform integrates with your existing systems, supporting more effective operations by automating and simplifying the referral process. Aidin’s team also rolls up their sleeves with your care management teams and post-acute providers to enable you to present patients with accurate, standardized metrics to operationalize informed decision-making.
Meeting transitions of care standards upstream with Aidin
The 2024 National IMPACT Assessment reflects an ongoing commitment to improving patient outcomes, care coordination, and transparency in healthcare. More than ever, providers are expected to adopt efficient, data-driven processes to comply with federal mandates. Aidin’s team and platform support you every step of the way. Our ROI-focused solutions help you meet CMS guidelines, but they also improve patient experience and operational efficiency while also meeting CMS guidelines.
Want to learn more about how Aidin can help your organization align with CMS standards, save money, and reduce administrative burden on your teams? Get in touch today.

