Overview
In November 2023, Aidin co-hosted a panel with two care management leaders to share how they’ve implemented cost-reducing changes that minimize administrative burden so their case management (CM) teams can focus on the important tasks that they are licensed to perform and can provide the best post-acute care options for their patients.
This white paper includes insights from a November 2023 webinar panel featuring these leaders:
- Steve Blau, Senior Director of Care Management and Transitional Care, Luminus Health
- Joanna Lucas, VP of Care Management, St. Luke’s University Health Network
Introduction
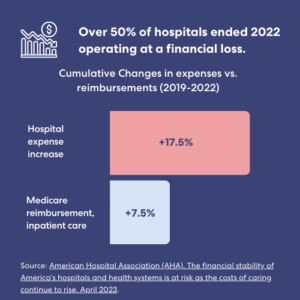
Unprecedented financial challenges threaten the sustainability of America’s hospitals and healthcare systems. According to an American Hospital Association report, at the end of 2022, over half of hospitals were operating at a financial loss. This is due to significant increases in the costs required to deliver patient care. Between 2019 and 2022, cumulative hospital expenses grew more than two times the cumulative increase in Medicare reimbursement for inpatient care.
The main drivers of hospital expenses are the rising cost of medical supplies and workforce shortages, which force hospitals to rely heavily on more expensive contract labor. Labor expenses have impacted hospital budgets heavily—contract rates charged to hospitals increased 56.8% in 2022 compared with pre-COVID-19 pandemic levels. Further, shortages in the workforce burden the clinical staff with administrative tasks that can lead to discharge delays, resulting in bed occupancies that are not reimbursed.
We gathered insights from care management leaders at two health systems on changing their case management staffing and processes to reduce costs and optimize patient care.
Setting up for success
Care management leaders face acute pressure to reduce costs while working with lower budgets and a shrinking workforce. Steve Blau, who directs Care Management at Luminis Health System, and Joanna Lucas, who oversees Care Management at St. Luke’s University Health Network, each uses forward-thinking strategies to tackle the financial pressures threatening the ability of their teams to operate at their highest level.
After evaluating their individual CM models, they each implemented similar fundamental changes that have not only introduced efficiencies and cost reductions but also positioned them with the flexibility required to meet potential challenges as healthcare delivery evolves.
Centralized support with standardized case management processes
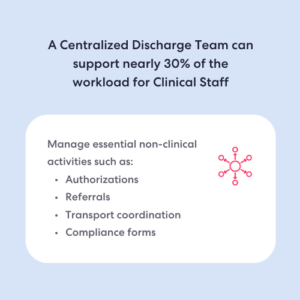
Both leaders adopted staffing and process changes designed to improve administrative efficiency while maintaining clinical excellence. Joanna Lucas estimated that prior to making changes, approximately one-third of her case managers’ workload consisted of administrative tasks that did not require a social worker or RN to perform.
An initial step both executives took was to assemble a centralized discharge planning team to focus on administrative aspects so case managers could focus on the clinical work for which they are trained. Their discharge planning teams are responsible for nonclinical yet critical activities such as referral management, authorizations, and transportation coordination. The team is solely focused on the administrative processes, so they have the capacity to monitor and follow up on delays.
Because they have proficient administrative teams supporting their clinical staff, both Steve and Joanna report that their CM workflows are more streamlined. Moreover, the discharge support teams were staffed using their existing budgets. Joanna evaluated and repurposed FTEs to hire six support staff who support 75 case managers across 11 acute care hospitals. And Steve leveraged the attrition of clinical staff to redirect funds for nonclinical paraprofessional positions.
Steve Blau quickly points out that workflow efficiency is more than centralizing resources. Standardizing processes is critical for the centralized team to truly support hospitals across the network. Process standardization is, therefore, performed in close collaboration with utilization management (UM). Further, Joanna Lucas created a position to serve as a point person for their standardization efforts. A case management educator focuses on ensuring that processes work for the entire network. They also monitor and evaluate competencies so department heads are not burdened with additional workflow-related responsibilities.
Leveraging technology for cost reduction & efficiency
Case management leaders have embraced technological solutions to streamline workflows, such as utilizing telehealth visits, ordering DME, and coordinating transport. However, technology also has potential value for further optimizing efficiency and reducing costs. Steve Blau believes that the right technology can be an accelerator if used judiciously, and both executives are exploring how to do just that. By identifying where real value can be added to their workflows, Joanna and Steve have been adopting technology-based tools to optimize processes.
Referral management was a key area of focus for Joanna Lucas. Specifically, she standardized the process with the Aidin platform’s help, which greatly impacted her ability to streamline referrals across 11 network hospitals successfully.
Both executives are using technology to obtain performance indicators for their post-acute providers. Steve Blau, who uses Aidin to do this, noted that the ability to access and evaluate performance data such as response times and acceptance and referral rates has been instrumental in improving their post-acute care transitions. In the two years since adopting Aidin, the platform has allowed them to establish a network of preferred providers based on performance. The hospital preferentially partners with providers who meet certain indicators while continuing to respect patient preferences.
Additionally, data obtained with Aidin allows Steve’s case management team to pinpoint potential pain points in internal workflows. This has been instrumental in making process adjustments so they can more effectively work with payers and post-acute providers.

Automation for cost reduction & time savings in case management
Automation is another way technology is evaluated as an effective cost-reduction tool. Joanna Lucas plans to automate manual, time-consuming steps in the UM workflow. By her estimation, the first process they plan to automate will likely save 20-25 hours a week in manual labor.
Joanna added that to be effective, technology solutions at St. Luke’s need to integrate with their EMR platform, Epic. Therefore, she works closely with her Epic team when adopting new platforms to ensure that they do not introduce additional complications that defeat the purpose of efficiency. For instance, case management teams can access the Aidin platform and Epic with a single sign-on step, which is an important consideration before introducing technology-based solutions.
Finally, utilizing AI-driven technology is an important consideration that case management leaders should have on their radar. Steve Blau noted that payers have embraced AI-driven tools for decision-making, so thinking strategically about how to use AI effectively is critical for case management success.
Building partnerships inside and outside the walls of hospitals
Close partnerships with post-acute providers can be instrumental in avoiding extended lengths of stay and ensuring that patients are discharged with appropriate follow-up care in place. Therefore, it’s unsurprising that Steve Blau and Joanna Lucas are developing strategies to preferentially partner with post-acute providers who can help them meet their patients’ needs.
Setting up a preferred network of high-performing providers is key to building strong partnerships with skilled nursing facilities (SNFs) in terms of cost and quality of care. Steve and Joanna use performance metrics, such as the response and acceptance rates that Aidin provides, to assess whether the provider can accommodate smooth transitions if they match their patient’s needs and requirements.
Both leaders have also made efforts to strengthen the relationship between CM and PT. Joanna Lucas collaborated with nurses and PTs to develop a standardized way to measure patient mobility, which has had a huge impact on length-of-stay. Steve Blau added that close, collaborative relationships between PT and CM are essential, given their overlapping roles.
Steve Blau also noted that, through collaboration with post-acute providers, he successfully launched a mobile integrated health solution that provides follow-up care for recently discharged patients. This helped him address gaps in care that often occur when patients are discharged to home care.
Finally, when considering partnerships, don’t ignore opportunities to optimize workflows by working more closely with internal teams. For instance, Steve Blau noted that his CM teams were overwhelmed by organizing patient follow-up visits until they leveraged features in Epic that made it easy for nurses to take on the responsibility.
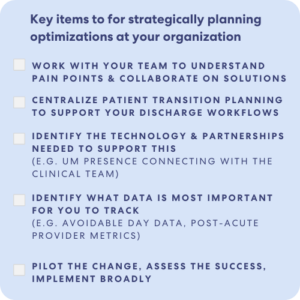
As care management leaders face unprecedented challenges to reduce costs while working with lower budgets and a shrinking workforce, Steve Blau and Joanna Lucas have demonstrated how fundamental changes can position case management teams for success.
Summary
Centralizing administrative tasks for discharge planning, optimizing processes, and building preferred partnering networks have introduced efficiency and reduced costs for both leaders. However, the role of technology in increasing efficiency cannot be underestimated. Leveraged correctly, technology-based solutions can improve patient transitions, reduce costs, and ensure patients receive the highest quality post-acute care.
Want to learn how your hospital or health system can leverage Aidin for similar cost reduction efforts?
Get in touch with our team for detailed data on cost reduction and time savings.

